A university team of physicians, veterinarians and animal behaviorists has begun research with two very special canines to sniff out cancer.
More info coming soon!
A university team of physicians, veterinarians and animal behaviorists has begun research with two very special canines to sniff out cancer.
More info coming soon!
Lung cancer is the No. 1 killer in the U.S., and more than 45,000 people will be diagnosed with head and neck cancer in 2015.
Early detection dramatically improves survival rates. Currently, no reliable methods exist to screen for these cancers.
Specially trained companion dogs can detect cancer with remarkable accuracy.
Please check out our Indiegogo page and find out more about how you can be a part of this amazing research!

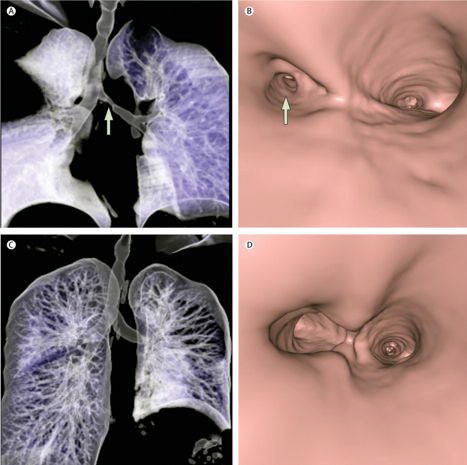
Manual control of the upper esophageal sphincter (UES) is possible with a simple implant placed on the cricoid cartilage. The swallow expansion device (SED) has been shown to increase UES opening to greater than normal proportions (Laryngoscope 2010 Apr;Suppl 1:S1-S16.). The SED is placed on the cricoid cartilage through a small cervical incision. Implantation takes the technical expertise and time required to perform a simple tracheotomy. A small post protrudes through the skin that, when pulled forward by the patient, opens the UES to super-physiologic proportions.
The device has proven safe and effective in eliminating aspiration in cadavers and in a large animal model of oropharyngeal dysphagia. Initial work in persons with swallowing dysfunction suggests that patients readily adapt to manual UES control. Training with the device is expected to be performed with the assistance of a speech and language pathologist under fluoroscopic guidance. The FDA has granted approval for a Phase I open label clinical trial on a limited number of patients with profound feeding tube dependent oropharyngeal dysphagia. If this initial investigation establishes that the device is safe and effective, the trial will be expanded to a larger cohort of persons with dysphagia.
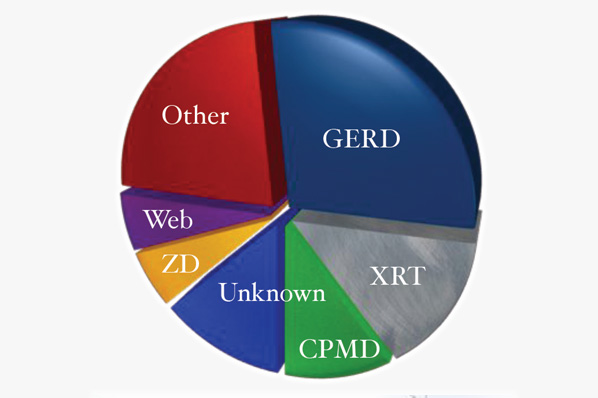
Dysphagia can be caused by innumerable disease processes. It has a significant impact on quality of life, life expectancy, and the utilization of health care resources. The most common causes of dysphagia have not been previously clarified. UC Davis CVS researchers led by Dr. Belafsky have published work that has documented the most common causes of swallowing difficulty in outpatient dysphagia sufferers (Ann Otol Rhinol Laryngol. 2013 May;122(5):335-8.).
Gastroesophageal reflux was the most common cause of swallowing impairment followed by radiation treatment for head and neck cancer and cricopharyngeus muscle dysfunction. Other less common causes of dysphagia identified by our team include esophageal dysmotility, progressive neurologic disease, hiatal hernia, eosinophilic esophagitis, vocal fold immobility, cervical spine surgery, and achalasia.
Interestingly, despite the most contemporary state-of-the-art diagnostic equipment, a source of the swallowing
complaint could not be identified in 13% of individuals. This highlights the need to differentiate between the subjective symptom of dysphagia and objective evidence of swallowing impairment and identifies room for improvement in our ability to diagnose tertiary causes of dysphagia.
These findings allow clinicians to better allocate health care resources and focus their research efforts to areas that provide maximum patient benefit and quality of life improvement.
Dr. Peter Belafsky and his team at the UC Davis Primate Center and University College London have received a $4.4 million grant from the California Institute of Regenerative Medicine (CIRM) to perform ground-breaking studies to help patients with complex airway disorders. The money will support pre-clinical work required to initiate a human clinical trial.
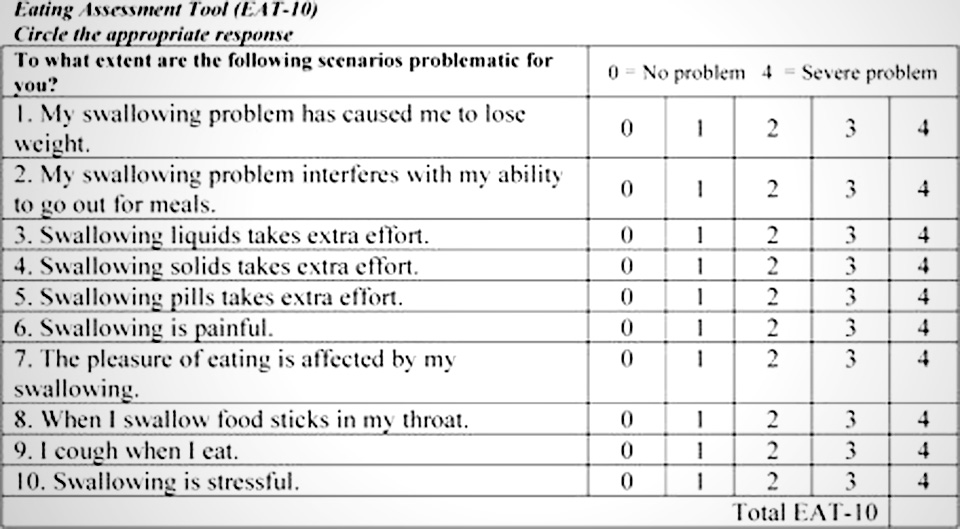
Dysphagia is a symptom, not a disease. Patients reporting the symptom of dysphagia may lack objective evidence of swallowing dysfunction. In order to accurately quantify the symptom of dysphagia, UC Davis CVS researchers have developed and validated a 10-item self administered survey instrument entitled the Eating Assessment Tool or EAT-10 (Ann Otol Rhinol Laryngol. 2008 Dec;117(12):919-24.).
The EAT-10 allows clinicians and scientists to document the degree of patient-reported swallowing-related disability as well as monitor dysphagia treatment efficacy. Normative data suggests that an EAT-10 ≥ 2 is abnormal. The instrument is becoming one of the most commonly used clinical research tools globally for persons with swallowing difficulty and is the primary outcome measure for dozens of investigations and clinical trials. The EAT-10 has been translated into numerous languages, including Japanese, Spanish, Anatolian Turkish, Italian, Chinese, and Portuguese.
Development of a pediatric version of the EAT-10 as well as a version to quantify the degree of swallowing difficulty for dogs and cats is currently underway.
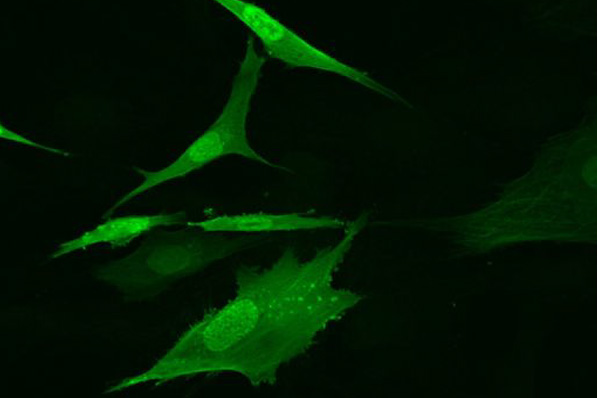
UC Davis CVS clinicians have embarked on an aggressive campaign to utilize regenerative medicine techniques to rehabilitate swallowing in patients with profound dysfunction. Recently published work from our center has shown that injected autologous muscle stem cells improve tongue strength in a large animal model of dysphagia (Laryngoscope. 2013 Aug 8.). We hope to begin a human clinical trial in the near future.
CVS researchers have discovered that suction placed below the upper esophageal sphincter can eliminate aspiration in a cadaver model of oropharyngeal dysphagia.
In work presented at the Dysphagia Research Society, our team has shown that catheters of various sizes placed retrograde up the esophagus through a gastrostomy eliminated 100% of barium aspiration in a cadaver model of profound oropharyngeal dysphagia.
Dr. Belafsky envisions a modified feeding tube with a dual function. The tube would serve as a traditional PEG tube for enteral nutrition. In addition, the tube would have an accessory catheter positioned retrograde up the esophagus at the level of the upper esophageal sphincter. The tube would be connected to a suction device affixed to a belt or clip. It could be placed in the office with a transnasal esophagoscope (TNE). The suction would assist with transport of a bolus from the pharynx (throat) into the esophagus. Once in the esophagus, the bolus would travel into the stomach by peristalsis and gravity.
Although our research has established proof of concept, challenges remain and a funding source for further prototype development has not been identified.
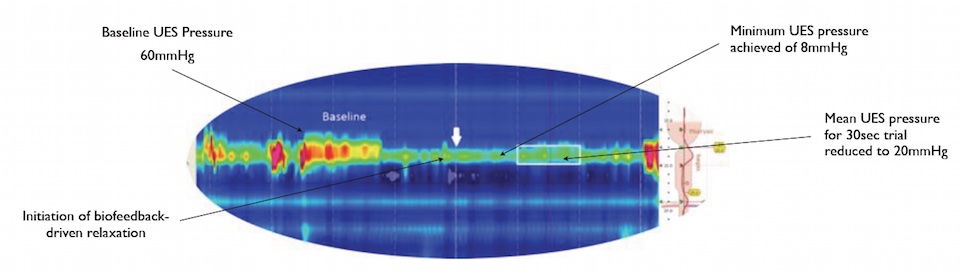
Drs. Kuhn and Belafsky have completed research that suggests that volitional control of the UES is possible with biofeedback. Patients with a high resolution manometry catheter in their pharynx who were placed in front of a biofeedback monitor were able to significantly increase and decrease their baseline UES pressure by 86 and 23 percent respectively. This work may have significant implications in the treatment of oropharyngeal dysphagia, gastroesophageal and laryngopharyngeal reflux, and globus pharyngeus.

Dysphagia is common and costly. Complications of swallowing dysfunction include dehydration, malnutrition depression, social isolation, pneumonia, pulmonary abscess, and death. For patients with profound disease,treatment options are limited. The UC Davis Center for Voice and Swallowing (CVS) is pushing the boundary of research and patient care.
CVS clinicians have established close collaborations with the UCD School of Veterinary Medicine, the UCD Institute for Regenerative Cures, The National Primate Center, The National Foundation of Swallowing Disorders, and the UCD Center for Health and the Environment. These collaborations have resulted in millions of dollars in grant funding, 4 patents, 2 startup companies, dozens of publications, 4 first in human and 5 first in canine surgeries. Our mission is to continue to advance the care of patients with disabling disorders of voice, swallowing, and breathing.