Care of the Professional Voice
Professional voice users have unique vocal needs that require special attention. Please note that glottal closure is complete and relaxed without any evidence of supraglottic involvement.
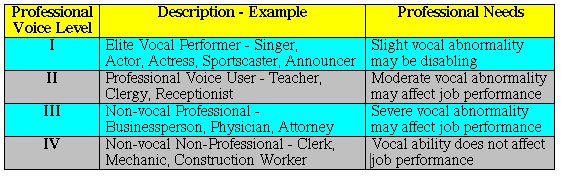
The disability caused by voice disorders is magnified tremendously when one’s livelihood depends on his or her ability to speak proficiently. In order to better treat professional voice users we have subclassified them into 4 separate categories which are listed in Table I.
Table I. Levels of Professional Voice Use
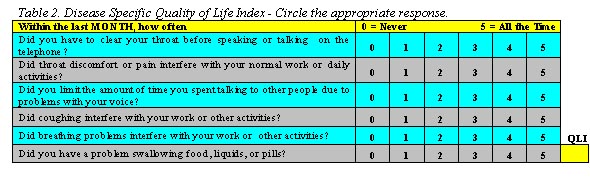
The professional voice level assists the clinician in formulating a treatment plan. Higher levels of vocal needs necessitate more aggressive treatment. In order to assess the severity of vocal disability we employ several survey tools. These instruments allow the clinician to document initial disease severity as well as assess treatment efficacy. We currently use the voice specific quality of life index (QLI), the voice handicap index (VHI), and a global assessment of overall health, the SF-12. The QLI is displayed in Table 2 below. A QLI greater than 5 indicates significant vocal disability.
Some of the most common disorders that affect professional voice users are infection (viral laryngitis), inflammatory disorders such as laryngopharyngeal reflux (LPR), medications (antihistamines, anxiolytics), tobacco smoke, smog and other environmental factors, neurologic disorders such as vocal fold paresis, and “so called” functional voice disorders (vocal fold misuse or abuse – see the article entitled The Demise of Functional Voice Disorders).
Frequently, several different factors act synergistically to produce the voice disorder. For instance, a classical singer with a voice specific QLI of 25 may have laryngopharyngeal reflux, allergies treated with a medication that causes drying of the mucous membranes, vocal fold paresis and second-hand exposure to tobacco smoke. Changing the patients medication or removing the second-hand smoke exposure may help somewhat (reduction in QLI to 15), but the patient will not experience maximal improvement (QLI < 5) until all factors are addressed and appropriately treated.
Our approach to the vocal professional with a voice disorder is to first establish the level of disability. This is accomplished by a comprehensive history, physical examination and administration of voice specific and global health indexes such as the voice handicap index (VHI), the voice-specific quality of life index (QLI), and the SF-12. The level of professional voice use is identified (Table I) and the vocal needs are tailored to a specific diagnostic and ultimate therapeutic protocol. Available diagnostics include stop motion videoendoscopy with stroboscopy, acoustic analysis with electroglottography, 24 hour pH monitoring to rule out LPR, and laryngeal electromyography to evaluate vocal fold paresis. Successful resolution of the voice disorder is accomplished only after each contributing factor has been identified and successfully treated.